Galactosemia

بیماری گالاکتوزمی
۳۰ آبان، ۱۴۰۱Other names of galactosemia
- Classic galactosemia
- Epimerase deficiency galactosemia
- Galactokinase deficiency disease
- Galactose epimerase deficiency
- Galactose-1-phosphate uridyl-transferase deficiency disease
- GALE deficiency
- GALK deficiency
- GALT deficiency
- UDP-galactose-4-epimerase deficiency disease
- UTP hexose-1-phosphate uridylyltransferase deficiency
- transferase deficiency galactosemia
General descriptions of galactosemia
Galactosemia is a rare inherited disorder of carbohydrate metabolism and interferes with the body’s ability to convert galactose to glucose. Galactose is the sugar in milk, such as breast milk and other dairy products. The human body also produces galactose, which is called endogenous galactose. Glucose is another type of sugar. In galactosemia, the body is unable to use galactose to generate energy. Researchers have identified several types of galactosemia, each of them being caused by a mutation in a specific gene and affecting various enzymes involved in the breakdown of galactose.
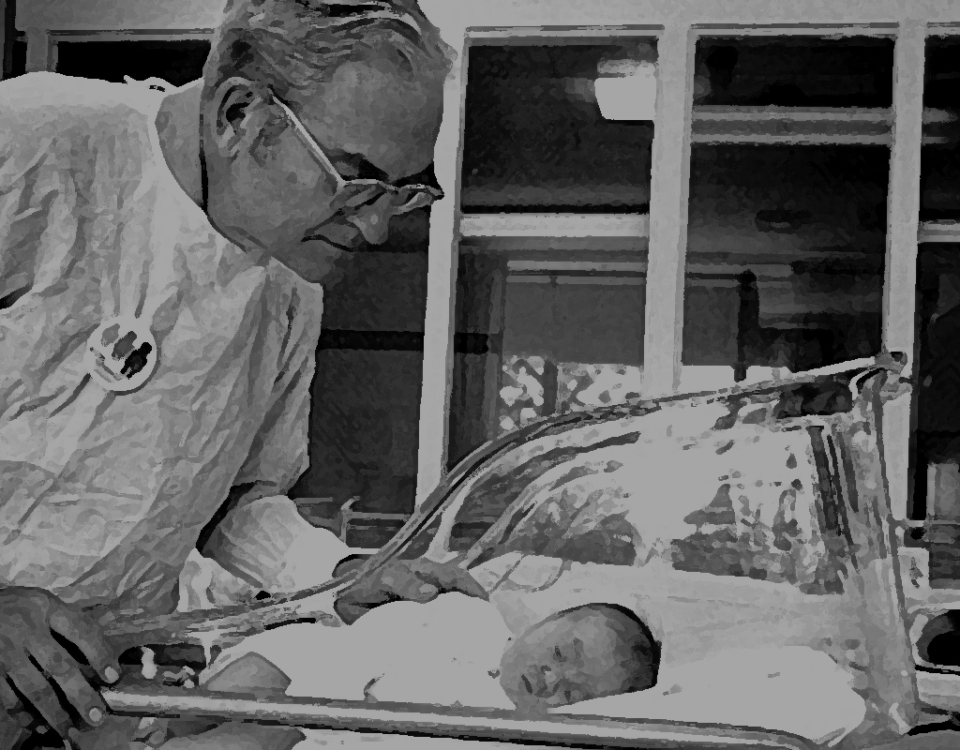
Classical galactosemia, also known as type I, is the most common and severe type of the condition. If infants with classic galactosemia are not treated quickly with a low-galactose diet, complications of the disease appear within days of birth. There are different signs and symptoms associated with Galactosemia type II (galactokinase deficiency) and type III (galactose epimerase deficiency). Type II galactosemia causes fewer medical problems than the classic type. Both classical galactosemia and clinical variant galactosemia can lead to life-threatening health problems unless lactose is removed from the baby’s diet soon after birth. Early diagnosis and treatment with a low-lactose diet (dairy-free) are vital to prevent mental retardation, liver failure, and death in infancy.
How is galactosemia transmitted?
Galactosemia is an autosomal recessive genetic disorder. Recessive genetic disorders occur when a person inherits a mutated gene from both parents. People who inherit one normal gene and one mutated gene will be carriers of the disease, and they usually won’t show any symptoms. The risk that the carrier parents will transmit the mutated gene and consequently have an affected child is 25% in each pregnancy. The risk of having a carrier child in each pregnancy is 50%. The chance of receiving normal genes for the child is 25%. The probabilities are the same for men and women.
Symptoms of galactosemia
Affected infants typically have feeding problems, lack of energy (lethargy), inability to gain weight and grow as expected (growth failure), yellowing of the skin and whites of the eyes (jaundice), liver damage, and abnormal bleeding. Other serious complications of this disease can include severe bacterial infections (sepsis) and shock. Affected children are also at risk for developmental delays, clouding of the lens of the eye (cataracts), speech problems, and mental retardation. Women with classic galactosemia may have fertility problems due to premature ovarian insufficiency. Signs and symptoms of type III galactosemia range from mild to severe and can include cataracts, developmental delay, mental retardation, liver disease, and kidney problems.
Causes of galactosemia
Mutations in GALT, GALK1, and GALE genes cause galactosemia. These genes provide the instructions for making enzymes required to process galactose obtained from the diet. These enzymes break down galactose into another simple sugar called glucose and other molecules that the body can store or use for energy. Mutations in the GALT gene cause classical galactosemia (type I). Most of these genetic changes almost destroy the activity of the enzyme produced by the GALT gene, preventing the proper processing of galactose and leading to the development of signs and symptoms of this disorder. Another mutation of the GALT gene, called the Duarte variant, reduces the enzyme’s function but does not eliminate it. People with Duarte type usually have milder symptoms of galactosemia.
Type II galactosemia is caused by mutations in the GALK1 gene, while mutations in the GALE gene cause type III galactosemia. Like the enzyme produced from the GALT gene, the enzymes produced from the GALK1 and GALE genes play an essential role in galactose processing. Deficiencies in any of these vital enzymes cause toxic levels of galactose and related compounds to build up in the body. The accumulation of these substances damages tissues and organs and leads to symptoms of galactosemia.
Prevalence of galactosemia
1 out of every 30,000 to 60,000 babies has classic galactosemia. Galactosemia types II and III are less common. Type II galactosemia affects less than 1 in 100,000 babies, and type III galactosemia is scarce.
Diagnosis of galactosemia
Classical galactosemia and clinical variant galactosemia are diagnosed when galactose-1-phosphate is high in red blood cells and GALT enzyme activity is reduced. Molecular genetic testing is also available to identify mutations in the GALT gene. Newborn screening using a blood sample from the baby’s heel can identify almost all newborns with galactosemia. If GALT enzyme activity is not measured, infants with clinical variant galactosemia may be missed in newborn screening.
Treatment of galactosemia
Infants with galactosemia should be on a lactose-restricted (dairy-free) diet that includes lactose-free milk substitutes and other foods such as soy. Children with galactosemia should not undergo a lactose tolerance test (L.T.T). Infants with galactosemia can synthesize galactolipids and other essential compounds containing galactose without the presence of galactose in food. Acceptable physical growth is quite possible if the child follows the diet. Speech therapy may be necessary for children with apraxia of speech or dysarthria. Individual education programs or professional help with learning skills may be required for some school-age children. It is also possible to use hormone replacement therapy for delayed puberty and premature ovarian insufficiency (POI). The emotional effects of a strict diet in children may require supportive measures during childhood.